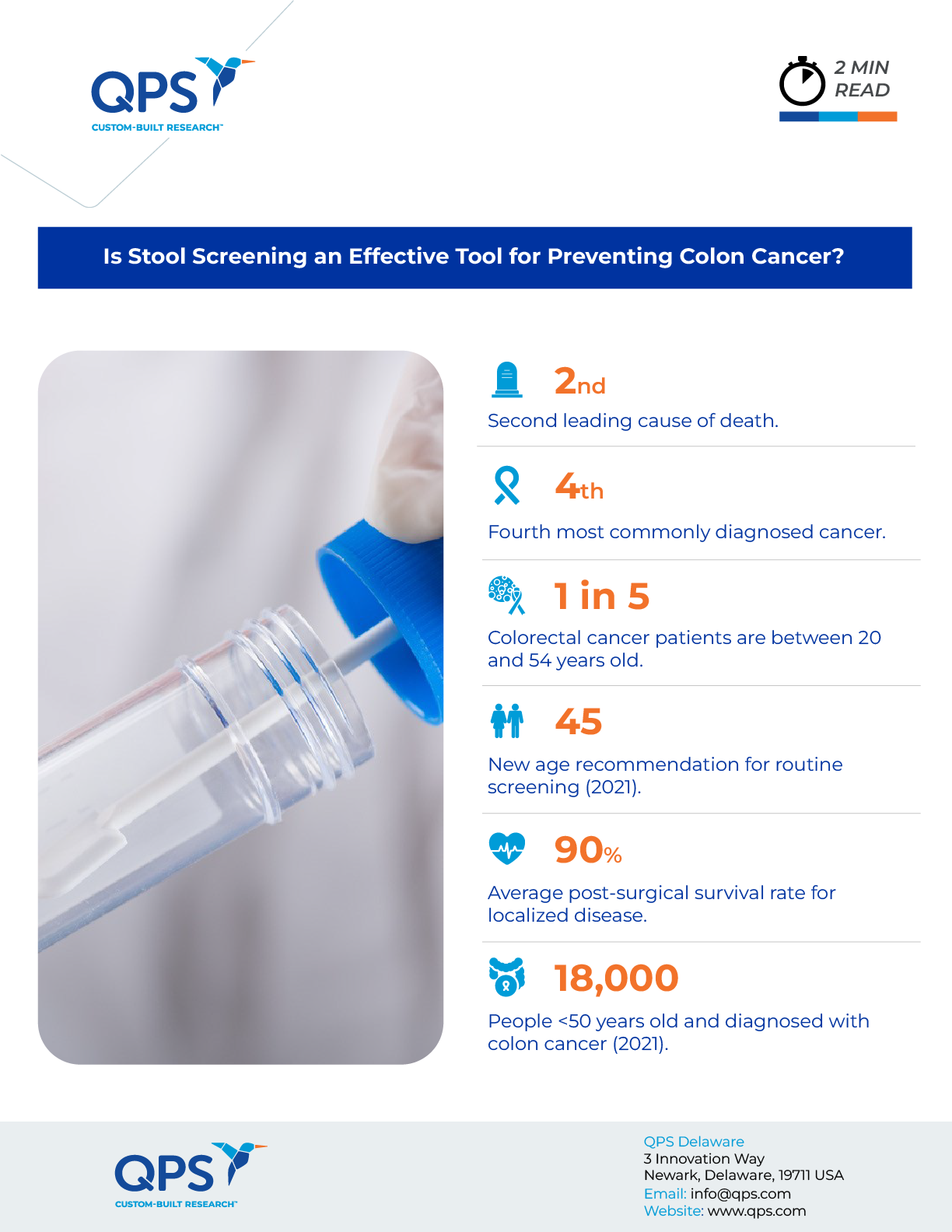
Colonoscopies have historically been the dominant method of screening for early detection of colon cancer, the third leading cause of cancer death in the United States for both men and women. However, recent research has not only challenged the conventional wisdom on the effectiveness of colonoscopies in reducing the risk of developing and dying from colon cancer but has also pointed towards stool screening as a potentially effective alternative method of screening for colon cancer.
Stool Screening vs. Colonoscopies
The two most highly recommended methods of screening for colon cancer are the fecal immunochemical test (FIT) and colonoscopies. The U.S. Preventative Services Task Force recommends both methods with no preference given to either.
With the FIT method, a small amount of stool is collected and analyzed for the presence of blood. If blood is detected, it may indicate the presence of colon cancer or other gastrointestinal conditions. The FIT method requires only one stool sample and does not require any dietary restrictions or changes beforehand. It can be performed at home and is significantly less invasive, less time-consuming, and less expensive than other screening methods, such as colonoscopy.
A colonoscopy, on the other hand, requires that the colon be emptied using a laxative. The procedure involves inflating the colon with air or carbon dioxide and inserting a flexible tube with a tiny camera to scan the entire rectum and colon for potentially cancerous growths. One of the benefits of a colonoscopy is that during the procedure, doctors are able to remove any potentially cancerous polyps they encounter.
Despite the significant differences in accessibility, invasiveness, and cost, in the United States, only 11 percent of adults over the age of 50 use stool screening. Conversely, 61 percent of the same age demographic report having a colonoscopy performed in the previous decade. This difference can be attributed to a significant push toward colonoscopies from health professionals. Colonoscopies have long been considered the gold standard in early detection. But with fewer than two-thirds of adults 45 and older getting the recommended regular colon cancer screenings, the focus on colonoscopies as the preferred method of screening has a serious problem: They don’t work if people don’t use them.
Christopher Almario, a gastroenterologist at Cedars-Sinai in Los Angeles, puts it this way: “A lot of times people think colonoscopy is synonymous with colorectal cancer screening. But a lot of people don’t want to do a colonoscopy.”
Rethinking Routine Screening Methods
Almario recently published a study examining the effectiveness of stool screening as an alternative method of early colon cancer detection. In his study, he educated unscreened adults about screening methods and then asked them to choose between an annual stool test and a colonoscopy, which is recommended every 10 years. The study found that when educated on their options, the majority of unscreened adults, and 77 percent of those 50 and older, preferred stool screening over colonoscopy as their preferred screening method for colon cancer.
Almario’s study raises important considerations about the potential benefits of educating the population about stool screening as an alternative to colonoscopies. While there are unique benefits to colonoscopies and potential downsides to stool screening, researchers believe there are legitimate reasons to consider alternatives to colonoscopies.
For one, for all of their benefits, colonoscopies are not risk-free procedures. Research shows that there are 14.6 major bleeding episodes and 3.1 colon perforations per 10,000 colonoscopies performed. Colonoscopies in the U.S. are also typically performed under sedation, which presents risks.
Recent studies have also indicated that the benefits of colonoscopies may not be quite as impressive as previously believed, with some analyses showing that colonoscopies reduced the risk of colon cancer and colon cancer death less than had previously been indicated.Researchers and scientists are clear: These studies and the risk factors of colonoscopies do not invalidate colonoscopies as a useful screening tool. Colonoscopies still have the advantage of reducing cancer incidence, which leads to fewer surgeries, chemotherapies, immunotherapies, and other treatments. Ultimately, scientists continue to stress the importance of regular colon screenings — whether with colonoscopies, FIT tests, or sigmoidoscopies, which are procedures using a tool that only examines a small portion of the colon — for those 45 and older.
However, this new research demonstrates that it may be time to reevaluate colonoscopies’ current standing as the gold standard of colon cancer screens. It also indicates that there may be a significant benefit in promoting and educating the public about alternative options that are less expensive and require less invasive tools, like stool screening, which may have more buy-in from the public. Ultimately, the goal is to increase the number of regular colon cancer screenings, which are critical in reducing colon cancer cases and fatalities.
QPS is a GLP- and GCP-compliant contract research organization (CRO) delivering the highest grade of discovery, preclinical and clinical drug research development services. Since 1995, it has grown from a tiny bioanalysis shop to a full-service CRO with 1,100+ employees in the U.S., Europe and Asia. Today, QPS offers expanded pharmaceutical contract R&D services with special expertise in neuropharmacology, DMPK, toxicology, bioanalysis, translational medicine and clinical development. An award-winning leader focused on bioanalytics and clinical trials, QPS is known for proven quality standards, technical expertise, a flexible approach to research, client satisfaction and turnkey laboratories and facilities. Through continual enhancements in capacities and resources, QPS stands tall in its commitment to delivering superior quality, skilled performance and trusted service to its valued customers. For more information, visit www.qps.com or email info@qps.com.