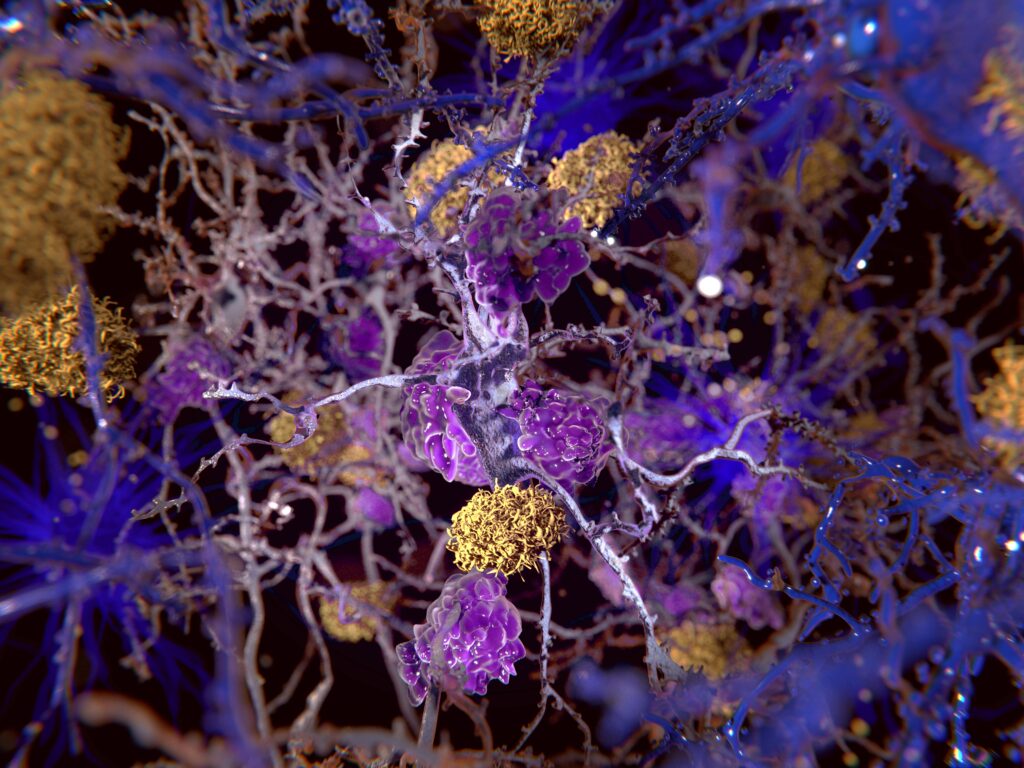
Alzheimer’s disease is a major global health concern: the devastating neurodegenerative disorder is responsible for 60-80 percent of all cases of dementia, and it affects 47 million people across the world. As scientists expect this number to continue to rise over the coming decades, the need for effective treatment options has never been more evident. There is currently no cure for Alzheimer’s disease, and available treatments only provide temporary relief of some symptoms. The lack of sufficient treatment options is owed, in large part, to unique challenges posed by the blood-brain barrier (BBB). Gene therapy for Alzheimer’s disease may offer a solution.
Alzheimer’s Disease Treatment Barriers
The search for effective Alzheimer’s disease treatments has been long and difficult, with Alzheimer’s disease drug trials historically encountering a 99-percent failure rate. The reasons for this failure rate are multi-faceted and complex, but one major hurdle that researchers have consistently encountered is the difficulty of developing treatments that can cross the blood-brain barrier (BBB). Gene therapy for Alzheimer’s disease, though, utilizes a more direct delivery system, bypassing the BBB altogether. That’s why, as the field continues to advance, many researchers are looking to gene therapy as a potentially promising approach to treating Alzheimer’s disease (AD) and other neurodegenerative conditions.
Exploring Gene Therapy for AD
Gene therapy for neurodegenerative disorders has made “straightforward progress” over the past two decades; researchers believe it has the potential to treat conditions such as AD, Parkinson’s disease, Huntington’s disease, and more. Gene therapy has the potential to accomplish this through multiple pathways, including direct correction of disease-causing genes, neuroprotection, neurorestoration, and control of symptoms.
Over the past two decades, researchers have assessed a range of different potential genetic targets for AD in preclinical trials, including amyloid pathway intermediates and enzyme modulation, tau protein downregulation, inflammatory cytokine alteration, APOE4 downregulation and APOE2 upregulation, and neurotrophin expression (nerve growth factor and brain-derived neurotrophic factor).
We’ll discuss two of these genetic targets in more detail below.
Brain-Derived Neurotrophic Factor (BDNF) Treatment
Brain-derived neurotrophic factor, or BDNF, is a protein responsible for promoting the survival of neurons and synapses in the central nervous system, particularly in the entorhinal cortex. In AD patients, levels of BDNF are reduced early in the progression of the disease.
Animal studies using adeno-associated virus (AAV2) to deliver BDNF to the entorhinal cortex of aged rats, aged monkeys, and amyloid mice showed promising results, with treated animals showing improvements in both learning and memory. In 2022, the first-in-human Phase I clinical trial investigating the safety and effectiveness of AAV2-BDNF gene therapy for AD patients officially began.
AAVrh.10-APOE2 Treatment
Apolipoprotein E, or APOE, is a gene expressed in three isoforms: APOE2, APOE3, and APOE4. APOE2 may offer protection against developing AD, while the APOE4 gene variant has a significant association with the risk of developing AD.
One approach that has drawn interest is the use of intrathecal administration of AAVrh.10-APOE2 (serotype rh.10 adeno-associated virus gene transfer vector expressing cDNA coding for human APOE2) to treat individuals who carry two copies of APOE4. This treatment aims to increase the expression of APOE2, which may help counteract the negative effects of APOE4.
In preclinical animal studies, the delivery of AAVrh.10-APOE2 directly into the brain resulted in widespread expression of APOE2, along with a decrease in beta-amyloid levels and amyloid deposition. A Phase I clinical trial examining LX1001 (AAVrh.10hAPOE2) is currently underway, involving 15 participants with confirmed amyloid deposition and a clinical diagnosis ranging from mild cognitive impairment to moderate dementia. The FDA granted Fast Track designation to this therapy in March 2022, and the trial is set to conclude in January 2024.
Looking Forward
While the use of gene therapy for Alzheimer’s disease treatment is a promising area of clinical research, there are still challenges affecting the ability to bring these therapies to market. These include the expensive and time-consuming subject screening and selection process, unreliable tools for longitudinal cognitive assessment, and a lack of support for decentralized clinical trials and remote monitoring of subjects. As technology continues to advance, however, researchers are hopeful that gene therapy may one day be a powerful tool in providing effective treatments for patients with Alzheimer’s disease.
QPS is a GLP- and GCP-compliant contract research organization (CRO) delivering the highest grade of discovery, preclinical and clinical drug research development services. Since 1995, it has grown from a tiny bioanalysis shop to a full-service CRO with 1,100+ employees in the U.S., Europe and Asia. Today, QPS offers expanded pharmaceutical contract R&D services with special expertise in neuropharmacology, DMPK, toxicology, bioanalysis, translational medicine and clinical development. An award-winning leader focused on bioanalytics and clinical trials, QPS is known for proven quality standards, technical expertise, a flexible approach to research, client satisfaction and turnkey laboratories and facilities. Through continual enhancements in capacities and resources, QPS stands tall in its commitment to delivering superior quality, skilled performance and trusted service to its valued customers. For more information, visit www.qps.com or email info@qps.com.