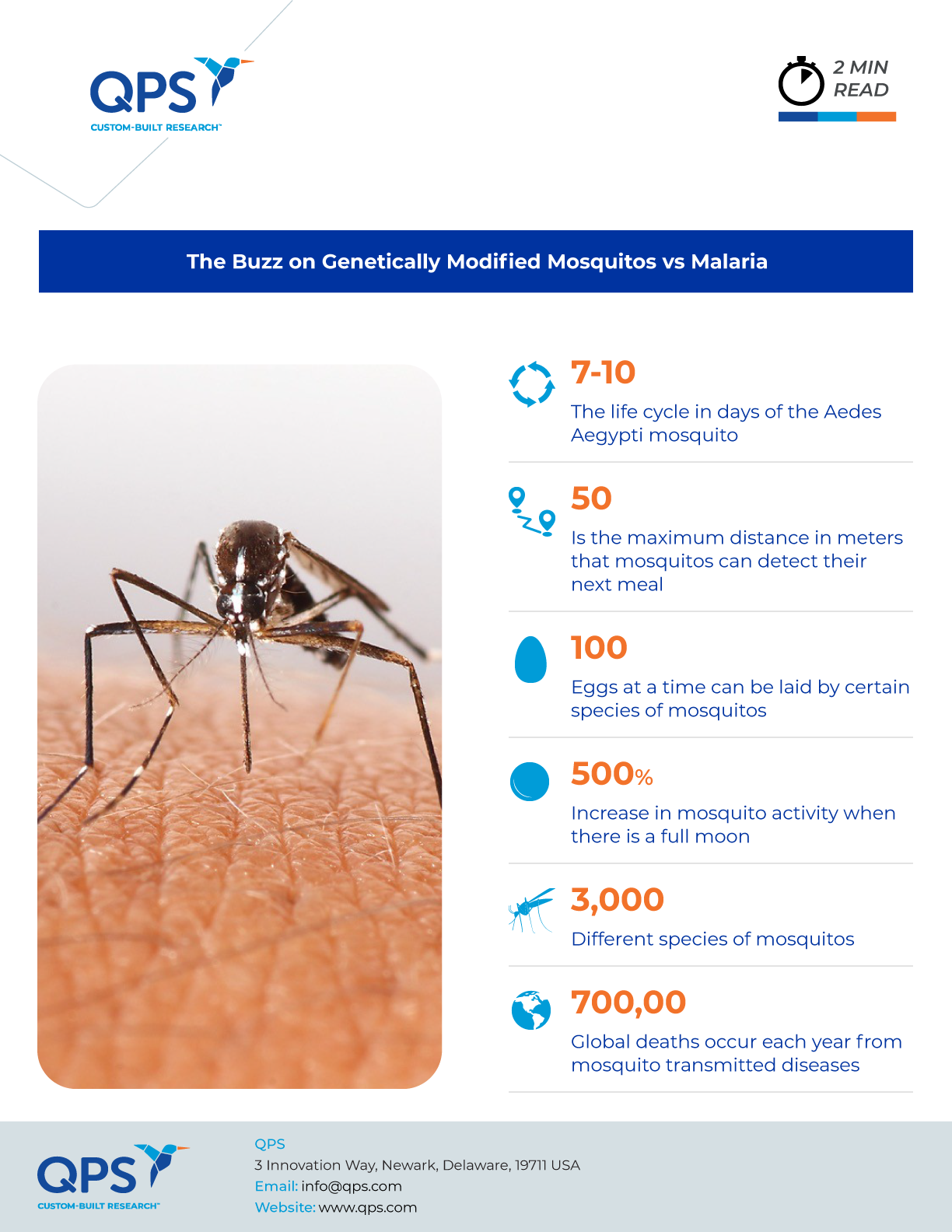
Malaria has been a devastating disease throughout history, claiming between 150 to 300 million lives in the 20th century alone. Despite significant progress in combating the disease, it remains a major threat, especially in African countries. The World Health Organization reported that there were 619,000 malaria deaths in 2021, with about 96 percent occurring in the WHO African Region and about 80 percent of those deaths occurring in children under age 5.
Although public health approaches focused on mosquito control have reduced malaria’s impact, it remains a persistent threat. “We’ve had great success over the past 20 years, using the bed nets and spraying, but those tools are not going to be enough to eliminate malaria,” said Gregory Lanzaro, director of the Vector Genetics Laboratory at the University of California, Davis. Researchers are now exploring a new approach to fight malaria by genetically modifying Anopheles mosquitoes, the disease’s primary vectors.
Gene Modification Challenges
Since the 1950s, scientists have been experimenting with various techniques to control the mosquito population, including using radiation to sterilize male mosquitoes and reduce their reproductive abilities. Researchers have also explored ways to reduce the lifespan of female mosquitos and make mosquitoes’ guts inhospitable to Plasmodium, the parasite that causes malaria. However, identifying a suitable genetic target for such goals has proven challenging, as gene functions are often complex, and changing them can lead to unintended consequences that may make it harder for the modified mosquitoes to survive in the wild long enough to spread the modified genes. These approaches, with decades of research behind them, have raised ecological and ethical concerns and present the challenge of being temporary. Over generations, the number of mosquitoes with the genetic alteration would gradually decrease as only half the offspring will inherit it.
The Game-Changer: Gene Drive
A game-changer in this effort is the concept of gene drive. This strategy uses portions of DNA — so-called selfish elements — that improve their own chance of being passed on to offspring. Researchers first considered the use of gene drive as a method to spread genes to control disease in the early 1990s. However, these elements could easily disrupt an organism’s genome, leading to early death.
Enter CRISPR-Cas9
The advent of CRISPR-Cas9 genome editing in 2012 transformed gene drive research. This tool allows for precise genetic sequence insertion, ensuring the transmission of a gene from one generation to the next indefinitely. Researchers have used CRISPR-Cas9 to develop gene drives in insects, such as fruit flies, and are now working to apply the tool in Anopheles mosquitoes to combat malaria. Different research teams are pursuing varying gene mutations, aiming to replace Plasmodium-carrying mosquitoes with disease-resistant ones or eliminate Anopheles mosquitoes entirely.
Population Replacement and Suppression
Some researchers are exploring population replacement, where modified mosquitoes spread disease-blocking mutations throughout the wild population. For example, molecular geneticist Anthony A. James at the University of California, Irvine, has led research using a gene drive to create modified mosquitos with antibodies to attack Plasmodium. Other investigators are using genetic engineering to try to suppress populations of mosquitos that carry the parasite. Jonathan Kayondo, a vector biologist who leads the research arm for Target Malaria in Uganda, prefers this population suppression approach to replacement due to the risk of parasite mutation. “With replacement, in a way, we are putting the pressure on the parasite to do something,” he says.
The Future of Gene-Modified Mosquitoes
Although other types of genetically modified mosquitos are currently used to control disease spread, those altered with gene drive will stay lab-bound while researchers assess the potential ecological impact of the technology. Some concerns involve the insect’s role in the food web and its possible effects on other insect populations and pollination.
To address ethical concerns and ensure local acceptance, researchers emphasize collaboration with African scientists and communities in malaria-affected regions. Engaging local stakeholders is seen as crucial for the success of gene-drive projects.
While gene drive technology shows promise, modified mosquitos represent just one tool that may eventually be deployed alongside current efforts. Together with insecticides, antimalarial drugs, and vaccines, researchers hope that genetically engineered mosquitos will someday help reduce malaria’s impact.
Did you enjoy this blog post? Check out our other blog posts as well as related topics on our Webinar page.
QPS is a GLP- and GCP-compliant contract research organization (CRO) delivering the highest grade of discovery, preclinical and clinical drug research development services. Since 1995, it has grown from a tiny bioanalysis shop to a full-service CRO with 1,100+ employees in the U.S., Europe and Asia. Today, QPS offers expanded pharmaceutical contract R&D services with special expertise in neuropharmacology, DMPK, toxicology, bioanalysis, translational medicine and clinical development. An award-winning leader focused on bioanalytics and clinical trials, QPS is known for proven quality standards, technical expertise, a flexible approach to research, client satisfaction and turnkey laboratories and facilities. Through continual enhancements in capacities and resources, QPS stands tall in its commitment to delivering superior quality, skilled performance and trusted service to its valued customers. For more information, visit www.qps.com or email info@qps.com.