Difficulty thinking, concentrating, and remembering are amongst the most debilitating long-haul symptoms of COVID-19. In some cases, this “brain fog” can linger for months. Of the first 100 patients with confirmed COVID-19 infections whose symptoms lasted at least six weeks, 81 reported experiencing brain fog. Until recently, the underlying causes of these lingering COVID-19 neurological symptoms have been a mystery. New research helps explain how SARS-CoV-2, the virus that causes COVID-19, spreads to the brain and why some patients experience severe neurological symptoms while others do not.
How SARS-CoV-2 Infiltrates the Brain
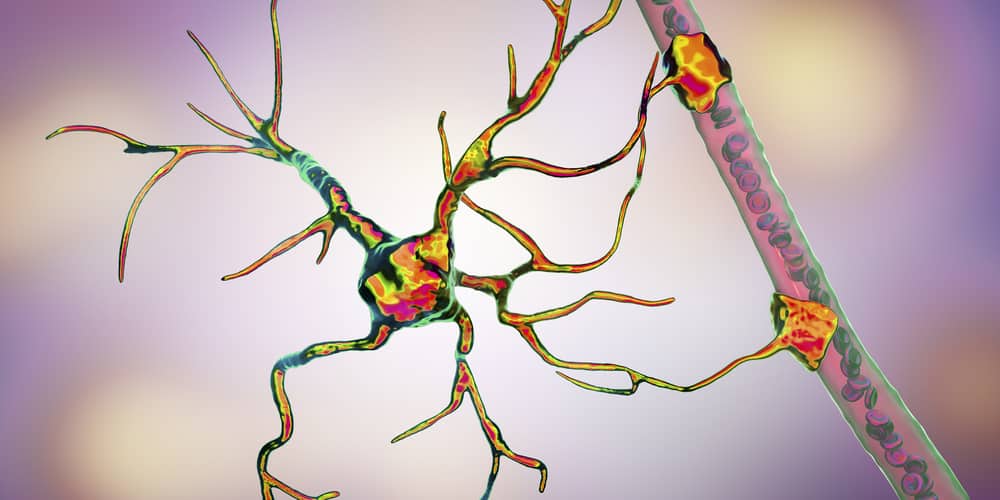
So, how does COVID-19 make its way into the brain? According to a new study led by Diana Cruz-Topete, assistant professor of molecular and cellular biology at Louisiana State University (LSU) Health Shreveport, SARS-CoV-2 is able to infect both neurons and astrocytes. Neurons are the nerve cells that transmit information between different areas of the brain, as well as other parts of the nervous system. Astrocytes are specialized, star-shaped glial cells that play many key roles in the nervous system, including protecting and supporting neurons.
The research suggests that SARS-CoV-2 uses astrocytes as pathways to the brain, where it causes damage that leads to neurological symptoms like brain fog, disorientation, loss of smell and taste, psychosis, and stroke.
The Role of ACE2 Receptors
In the respiratory system, scientists are aware that SARS-CoV-2 infects cells by attaching to the angiotensin-converting enzyme-2 (ACE2) receptors on the cell surface. For this study, the researchers wanted to determine whether ACE2 receptors played a role in the nervous system as well.
Cruz-Topete conducted the study in collaboration with Oscar Gomez-Torres, PhD, and Emma Burgos-Ramos, PhD, from Universidad de Castilla-La Mancha in Spain. The research team examined RNA and proteins to assess whether cell cultures of human astrocytes and neurons expressed ACE2 receptors. After that, the team exposed the cells to a version of the SARS-CoV-2 virus that had been modified to ensure the researchers’ safety.
The study established that both astrocytes and neurons express ACE2 receptors and are able to be infected with SARS-CoV-2. However, astrocytes and neurons are not equally vulnerable to SARS-CoV-2 infection, which may explain why some patients experience more significant neurological symptoms than others.
Why Do Some Patients Experience Severe COVID-19 Neurological Symptoms?
Although astrocytes and neurons are both able to be infected by SARS-CoV-2, astrocytes are less susceptible to infection. However, astrocytes present a bigger risk because they are the primary gateway to the brain, responsible for transporting nutrients from the bloodstream to the neurons. If astrocytes become infected with SARS-CoV-2, they can easily transfer the virus to a multitude of neurons in the brain.
According to the researchers, the fact that astrocytes present a higher risk than neurons may explain why some patients present very few neurological symptoms, if any, while others have severe neurological symptoms. Even if only a few astrocytes are infected in a patient, the infection can quickly spread within the brain. Fortunately, astrocytes have a higher resistance to infection, making severe neurological symptoms less likely.
Did you enjoy this blog post? Check out our other COVID-related blog posts as well as related topics on our Webinar page.
QPS has CLIA-certified and GLP-compliant laboratories ready to fast-track your novel coronavirus and COVID-19 RT-qPCR/QPCR and Serological Assays and vaccine development programs. Since 1995, QPS has provided discovery, preclinical, and clinical drug development services. An award-winning leader focused on bioanalytics and clinical trials, QPS is known for proven quality standards, technical expertise, a flexible approach to research, client satisfaction, and turnkey laboratories and facilities. For more information, visit www.qps.com/coronavirus or email covid19study@www.qps.com.







