Like most viruses, SARS-CoV-2 infects its hosts by entering and “hijacking” the operations of a host cell. A significant amount of the research on COVID-19 has focused on how the virus’s surface spike protein works as a means to develop treatment and preventive measures like the vaccines. But that isn’t the only area of interest – other studies focus on how the virus enters a cell, integrates its RNA with the host genome, and exits, with hopes of determining different ways to fight the spread of COVID-19. A recent article in Nature reviewed research on the virus since its emergence in late 2019 and includes some of these studies.
In part one of this series, we looked at the three-hinged flexibility of the SARS-CoV-2 spike protein as one factor that makes the virus particularly infectious. Here in part two, we will examine the events that occur after the virus has attached to a human host cell. While there is still a lot to learn about this interaction, recent studies are making some functions clearer.
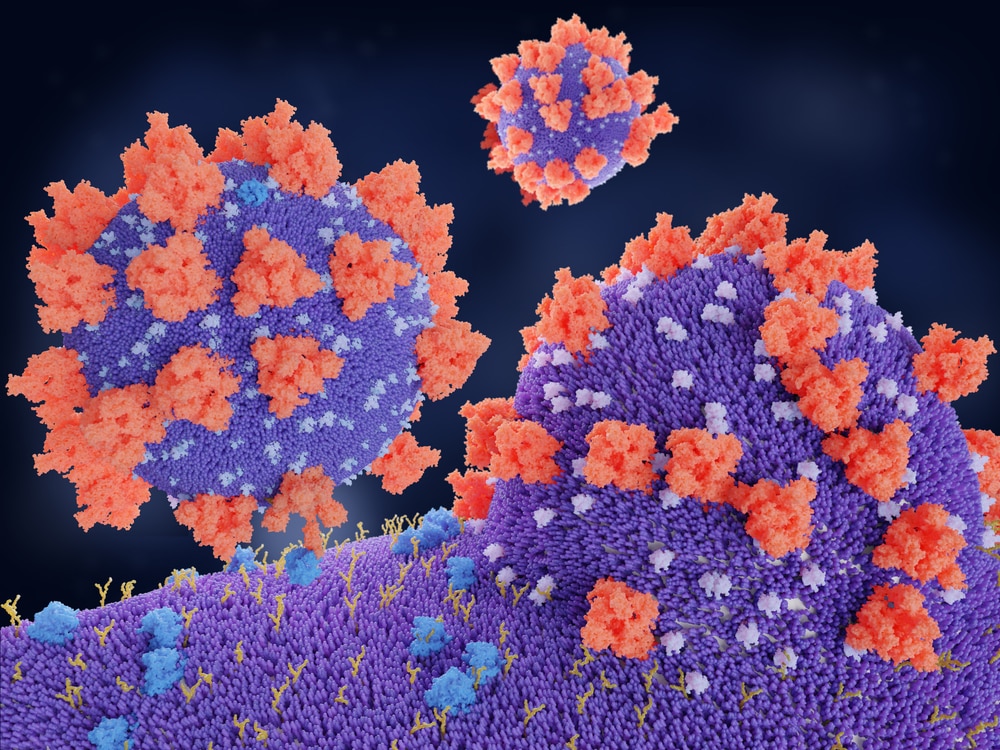
A Viral Merger
The binding of the SARS-CoV-2 spike to the host cell’s ACE2 receptor triggers a molecular reaction that merges the viral and cell membranes, opening the door for the virus’s RNA to enter. In this reaction, the virus uses a host protease, TMPRSS2, that cleaves a site on the spike protein’s Subunit 2 (S2). The cleavage exposes hydrophobic amino acids in the spike that enter the host cell membrane. Then, the spike folds into itself, making the viral and cell membranes fuse – a process that increases the speed of infection. This process is different from SARS-CoV, which bypassed TMPRSS2 in favor of another protein, called cathepsin. SARS-CoV-2’s route avoids using endosomes to enter a host cell, where it could encounter antiviral proteins and be trapped.
Once in the cell SARS-CoV-2 behaves like most viruses: the RNA genome is translated through host cell ribosomes, creating RNAs that code for more than two dozen viral proteins. The virus then creates its own messenger RNA while suppressing host cell mRNA to give the virus the advantage. While these steps are typical of any infectious virus, SARS-CoV-2 seems particularly efficient in its ability to take over protein expression, quickly making viral spike proteins and the other structures that make up the SARS-CoV-2 virus.
A Hint at Possible Preventive Measures
The process that SARS-CoV-2 uses to insert its genome into the host cell indicates that protease inhibitors could prevent the virus from utilizing TMPRSS2 or any other protease, and act as a powerful antiviral treatment. “We should have such protease inhibitors as broad antivirals available to fight new disease outbreaks and prevent future pandemics at the very beginning,” said Stefan Pöhlmann, researcher at the German Primate Center in Göttingen and a leader in research on ACE2 and TMPRSS2.
“Known Unknowns” Guide Additional Research
Just as this new insight has already provided a path to explore in preventive measures, research continues to fully understand what happens inside the host cell and how interfering with those processes could thwart viral translation:
- The virus (like other coronaviruses) turns the endoplasmic reticulum into a double-membrane sphere, forming a barrier from immune sensors and possibly allowing a haven for replication of viral RNA. Researchers are looking into how antiviral medicines might target the proteins that make these spheres.
- It is still not known exactly how SARS-CoV-2 exits the host cell. Most viruses either use their outer envelope or the Golgi complex – organelles that package molecules in membranes – to exit, but research shows this is not the case for SARS-CoV-2. Researchers at NIH are now exploring lysosomes as likely exit vehicles and are testing inhibitors as possible antiviral drugs.
- Other data points that researchers are working to determine include the number of ACE2 receptors needed to bind to each spike protein; at what point the S2 site is cleaved by TMPRSS2; and the number of spikes needed for virus-cell membrane fusion. Knowing any of these details could help determine ways to interrupt the replication process.
As researchers learn more about how the SARS-CoV-2 virus enters and exits the cell, the scientific community can identify additional ways to stop or interrupt these processes that enable the spread of COVID-19.
In the next part of this series, we will review the known variants and the latest research on their biology and infectivity.
Did you enjoy this blog post? Check out our other COVID-related blog posts or features on our Webinar page.
QPS is a CLIA-certified GLP- and GCP-compliant contract research organization (CRO) delivering the highest grade of discovery, preclinical and clinical drug research development services. Since 1995, it has grown from a tiny bioanalysis shop to a full-service CRO with 1,100+ employees in the U.S., Europe and Asia. Today, QPS offers expanded pharmaceutical contract R&D services with special expertise in neuropharmacology, DMPK, toxicology, bioanalysis, translational medicine and clinical development. An award-winning leader focused on bioanalytics and clinical trials, QPS is known for proven quality standards, technical expertise, a flexible approach to research, client satisfaction and turnkey laboratories and facilities. Through continual enhancements in capacities and resources, QPS stands tall in its commitment to delivering superior quality, skilled performance and trusted service to its valued customers. For more information, visit www.qps.com or email info@qps.com.




