Results of a comprehensive global study of antimicrobial resistance (AMR) show that infections caused by antibiotic-resistant bacteria — also known as “superbugs” — were among the leading causes of death in 2019, killing more people than HIV/AIDS or malaria.
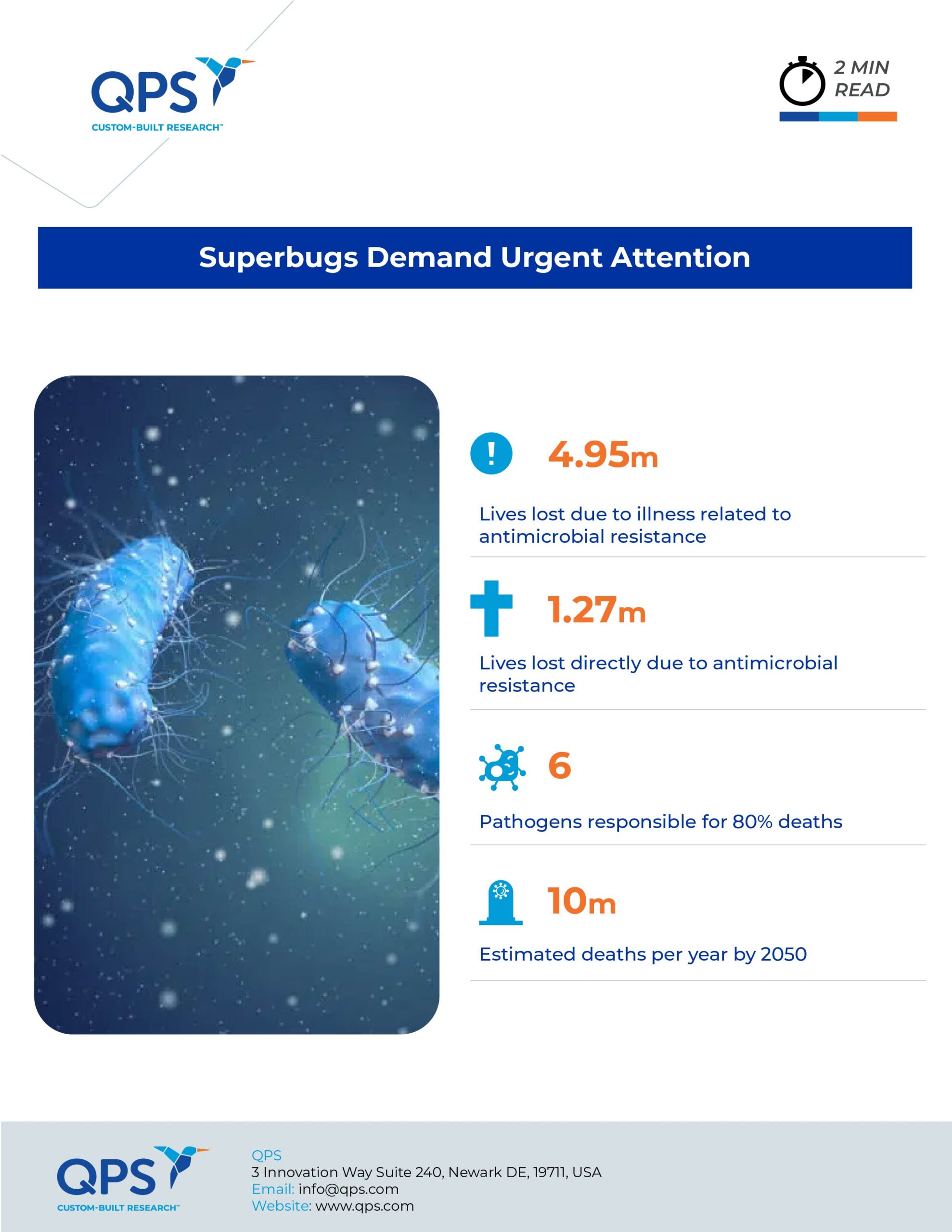
The report, published in the Lancet in January, estimates that 4.95 million people died from illnesses related to AMR and that 1.27 million of these deaths were a direct result of AMR. Additionally, the proportion of bacteria that is antibiotic-resistant is increasing. A 2016 report commissioned by the UK Prime Minister estimated that AMR may cause as many as 10 million deaths per year by 2050.
A Comprehensive Approach
The new study stands out for its global scope. The researchers started with information from the 2019 Global Burden of Diseases, Injuries, and Risk Factors Study (GBD), which estimates the prevalence of 369 diseases and injuries in 204 countries and territories in 1990–2019. This provided an estimate of the number of infection-related deaths globally and the pathogens responsible. To determine the total impact of AMR, they applied all available AMR data, including information from hospital and laboratory records, systematic literature reviews, surveillance systems, and clinical trials, to the GBD estimates.
They calculated the disease burden for 23 pathogens and 88 pathogen-drug combinations based on two counterfactual scenarios: one in which all drug-resistant infections were replaced by drug-susceptible infections, and one in which all drug-resistant infections were replaced by no infection. With this approach, the researchers estimated the difference between the burden associated with resistance and the burden attributable to resistance.
Deadliest Infections
Infections in the chest, bloodstream and abdomen accounted for 78.8% of the deaths that were directly attributable to AMR. Lower respiratory infections were responsible for more than 1.5 million resistance-associated deaths, more than any other type of infection. Six pathogens were responsible for almost 80% of the 1.27 million deaths directly caused by AMR: Escherichia coli, Staphylococcus aureus, Klebsiella pneumoniae, Streptococcus pneumoniae, Acinetobacter baumannii, and Pseudomonas aeruginosa.
Geographic Disparities
The prevalence of AMR and rates of resistance-related deaths are higher in lower-income countries, with the highest rate of deaths directly related to AMR in Western sub-Saharan Africa (27.3 deaths per 100,000). Australasia had the lowest rate (6.5 deaths per 100,000). The disparity between low- and high-income countries is due to differences in sanitation and hygiene, facilities for testing and a lack of access to the latest antibiotics and vaccines.
Regional Response
The study authors propose that targeted approaches are necessary when responding to the threat of AMR. They note that, although proper management of antibiotic use is important, limiting access to antibiotics is not appropriate in all settings. For example, they suggest that in western sub-Saharan Africa, increased access to antibiotics would save lives and decrease the AMR burden when second-line antibiotics are unavailable. In South Asia, where antibiotic overuse or misuse is a problem, restricting access to antibiotics might be appropriate.
Estimates from the analysis could be used to improve treatment guidelines. For example, the authors suggest that their data could be used to determine the dominant bacterial pathogens for a particular infectious syndrome and the antibiotics that would be most effective.
Infrastructure Needed
The researchers conclude that the findings “clearly show that drug resistance in each of these leading pathogens is a major global health threat that warrants more attention, funding, capacity building, research and development, and pathogen-specific priority setting from the broader global health community.” They call out the critical need for laboratory infrastructure to respond to this threat. This would improve and expand AMR surveillance and research. As the study authors stated, “Identifying strategies that can work to reduce the burden of bacterial AMR — either across a wide range of settings or those that are specifically tailored to the resources available and leading pathogen–drug combinations in a particular setting — is an urgent priority.”
Did you enjoy this blog post? Check out our other blog posts as well as related topics on our Webinar page.
QPS is a GLP- and GCP-compliant contract research organization (CRO) delivering the highest grade of discovery, preclinical and clinical drug research development services. Since 1995, it has grown from a tiny bioanalysis shop to a full-service CRO with 1,100+ employees in the U.S., Europe and Asia. Today, QPS offers expanded pharmaceutical contract R&D services with special expertise in neuropharmacology, DMPK, toxicology, bioanalysis, translational medicine and clinical development. An award-winning leader focused on bioanalytics and clinical trials, QPS is known for proven quality standards, technical expertise, a flexible approach to research, client satisfaction and turnkey laboratories and facilities. Through continual enhancements in capacities and resources, QPS stands tall in its commitment to delivering superior quality, skilled performance and trusted service to its valued customers. For more information, visit www.qps.com or email info@qps.com.