In human cells infected by the human immunodeficiency virus (HIV), virus particles can leave behind part of their genetic material, which gets incorporated into the cellular DNA. Known as provirus, this genetic material can persist indefinitely in infected human cells and can lead to resurgence of the disease.
Using cutting-edge gene-sequencing technology to analyze HIV genetic material from people on long-term antiretroviral therapy (ART), researchers observed that the virus hides its DNA in remote stretches of the human genome known as “gene deserts.” Continued analysis of these gene deserts may help researchers develop a strategy to permanently stop the virus.
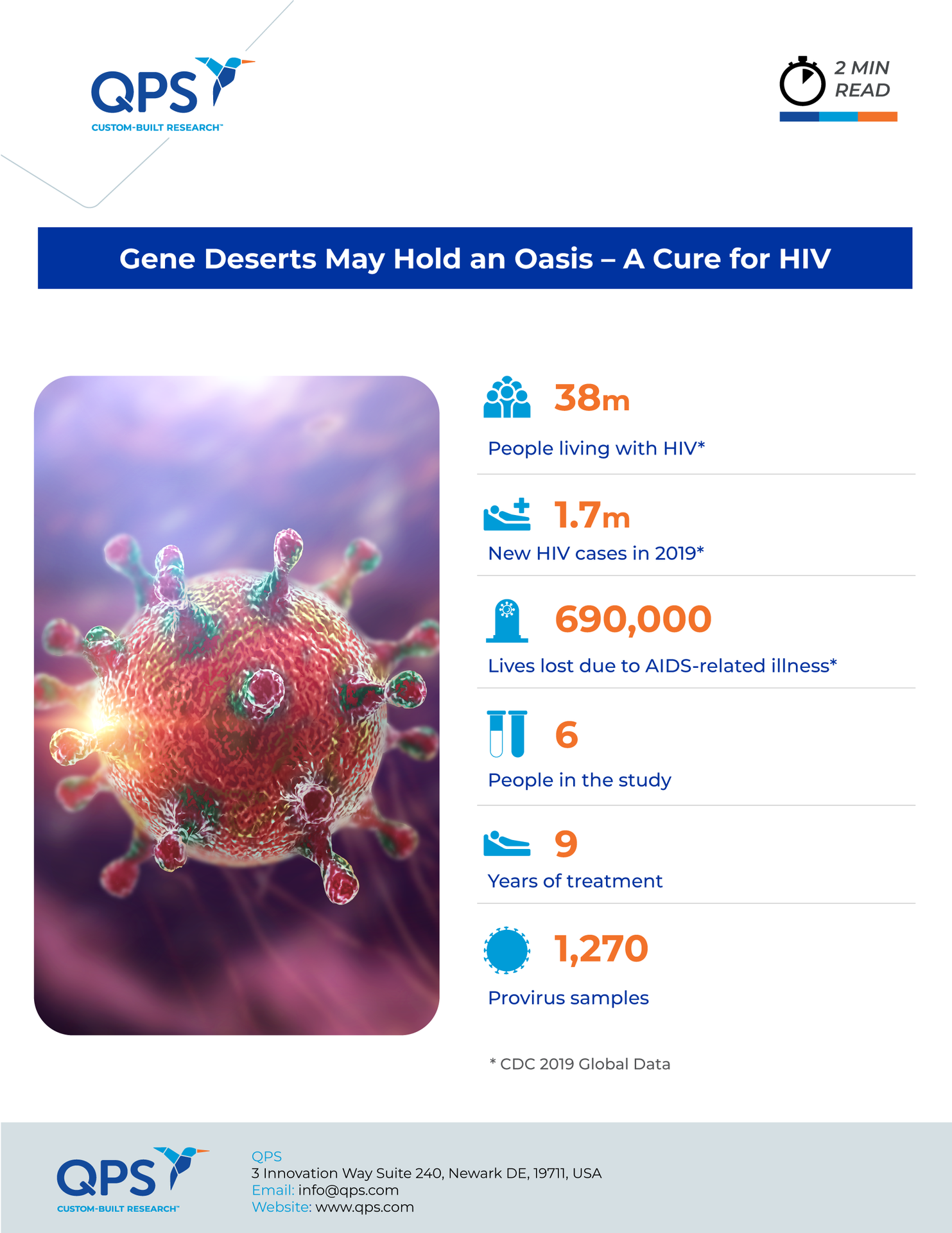
The new research, published in Cell in January, analyzed proviral material from six people with HIV who had been on treatment for at least nine years. The research team was led by spouses Xu Yu and Mathias Lichterfeld at the Ragon Institute, a collaboration between Harvard University, the Massachusetts Institute of Technology, and Massachusetts General Hospital. They reported that the proviruses that endure the longest tend to stay trapped in largely inactive stretches of human DNA. This entrapment could be preventing new viruses from being produced.
Can HIV Be “Blocked and Locked”?
A very small group (less than 0.5%) of people infected with HIV live with the virus for decades without treatment and remain asymptomatic. Researchers have studied this group of “elite controllers” for hints about the mechanism behind this inherent protection and how medicine might mimic it.
As the Ragon Institute reported in 2020, proviruses in these cases tend to hide out in regions of chromosomes that either don’t have genes or are home to mostly inactive genes that code for a type of protein known as a zinc finger (ZNF). In both cases, the DNA is especially tightly packed compared to other regions of the genome, making proviruses less accessible to factors needed for transcription. Then, in a 2021 paper, the researchers suggested that, when HIV becomes integrated into such regions, it does not go silent but rather produces a minimal amount of new virus that is eliminated by the immune system. HIV is technically active in these reservoirs, but it is effectively “blocked and locked.”
The recent publication reports on the researchers’ analysis of 1,270 provirus samples taken at various times during prolonged treatment. In three of the six people, intact HIV genes gathered in the remote DNA regions and dormant ZNF genes. In these cases, the virus integrated into the human DNA in a way that resembles what researchers have observed in the elite controllers.
Potential Clues to a Cure
Similar results have emerged from research led by Lillian Cohn, an immunologist at the Fred Hutchinson Cancer Center. Among people on ART for four to 21 years, the analysis showed that HIV proviruses were also clustered in certain ZNF genes.
Scientists don’t yet know why HIV DNA ends up there. They suggest it could be happenstance or the ZNF proteins may be actively involved. The big question going forward is whether a medical intervention could trigger this response. “It doesn’t necessarily need to be that people are somehow elite and special, but, rather, we might be able to induce this same phenotype in other people,” Cohn said.
Researchers have proposed several potential mechanisms. Suggestions include using drugs to target the HIV DNA and disrupt the transcription process, as well as vaccines that would spur the immune system to eliminate the proviruses faster.
Is it Safe to Stop Treatment?
The researchers think that people who have received treatment for a long time and have demonstrated the “blocked and locked” form of genetic integration may be able to stop treatment. They plan to test the strategy soon in “treatment-interruption” studies. A new initiative is underway to find and enroll people who have been on ART for decades and may be good candidates for stopping treatment with careful analysis and monitoring.
Dawn Averitt, who has remained healthy with HIV and has taken ART for more than 20 years, says that if she turns out to be a good candidate for such a study, she will probably volunteer. “I figured out how to do the dance with these drugs, but I really care what it means for all of us,” she says. “Imagine the hope, imagine the possibility, of being able to say, ‘Worry about keeping it under control now, don’t worry about what this means forever.’”
Did you enjoy this blog post? Check out our other blog posts as well as related topics on our Webinar page.
QPS is a GLP- and GCP-compliant contract research organization (CRO) delivering the highest grade of discovery, preclinical and clinical drug research development services. Since 1995, it has grown from a tiny bioanalysis shop to a full-service CRO with 1,100+ employees in the U.S., Europe and Asia. Today, QPS offers expanded pharmaceutical contract R&D services with special expertise in neuropharmacology, DMPK, toxicology, bioanalysis, translational medicine and clinical development. An award-winning leader focused on bioanalytics and clinical trials, QPS is known for proven quality standards, technical expertise, a flexible approach to research, client satisfaction and turnkey laboratories and facilities. Through continual enhancements in capacities and resources, QPS stands tall in its commitment to delivering superior quality, skilled performance and trusted service to its valued customers. For more information, visit www.qps.com or email info@qps.com.