A potential new cancer drug delivery method — through the gut’s lymphatic system rather than blood vessels — could improve treatment outcomes and reduce side effects while decreasing drug resistance.
Researchers from the University of Michigan demonstrated the strategy in mice, using LP-182 – a drug designed to simultaneously inhibit phosphoinositide 3-kinase (PI3K) and mitogen-activated protein kinase (MAPK). These kinases are intermediate signaling molecules that are part of a pathway implicated in the development of many types of cancer.
Although PI3K inhibitors have been approved to treat leukemia and lymphoma, interest has dimmed due to drug toxicity. In June, the FDA issued a warning about possible increased risk of death and serious side effects for Secura Bio’s PI3K inhibitor Copiktra® (duvelisib), which earned approval in 2018 to treat relapsed or refractory chronic lymphocytic leukemia (CLL) or small lymphocytic lymphoma (SLL). The warning came after the company released confirmatory Phase III trial results. Recently, after reviewing data from patients followed-up after participating in clinical trials, safety concerns led the agency’s Oncologic Drugs Advisory Committee to vote against use of the drug for chronic CLL and SLL previously treated with at least two therapies. In addition, Secura, Gilead, and Incyte withdrew their accelerated approvals for their PI3K inhibitors after failing to complete confirmatory trials. The FDA now requires randomized trials for PI3K inhibitors in blood cancers.
Finding the Right Balance
Combination therapy, using two or more therapeutic agents, for cancer is designed to target different cancer cell vulnerabilities. Because most oral drugs are absorbed through the blood, they first pass through the liver and can be metabolized at different rates. This can make it difficult to maintain the correct concentration of each drug in a balance that will have the intended therapeutic effect without causing side effects. It can also lead to drug resistance as the molecular pathways adapt to resist the therapy.
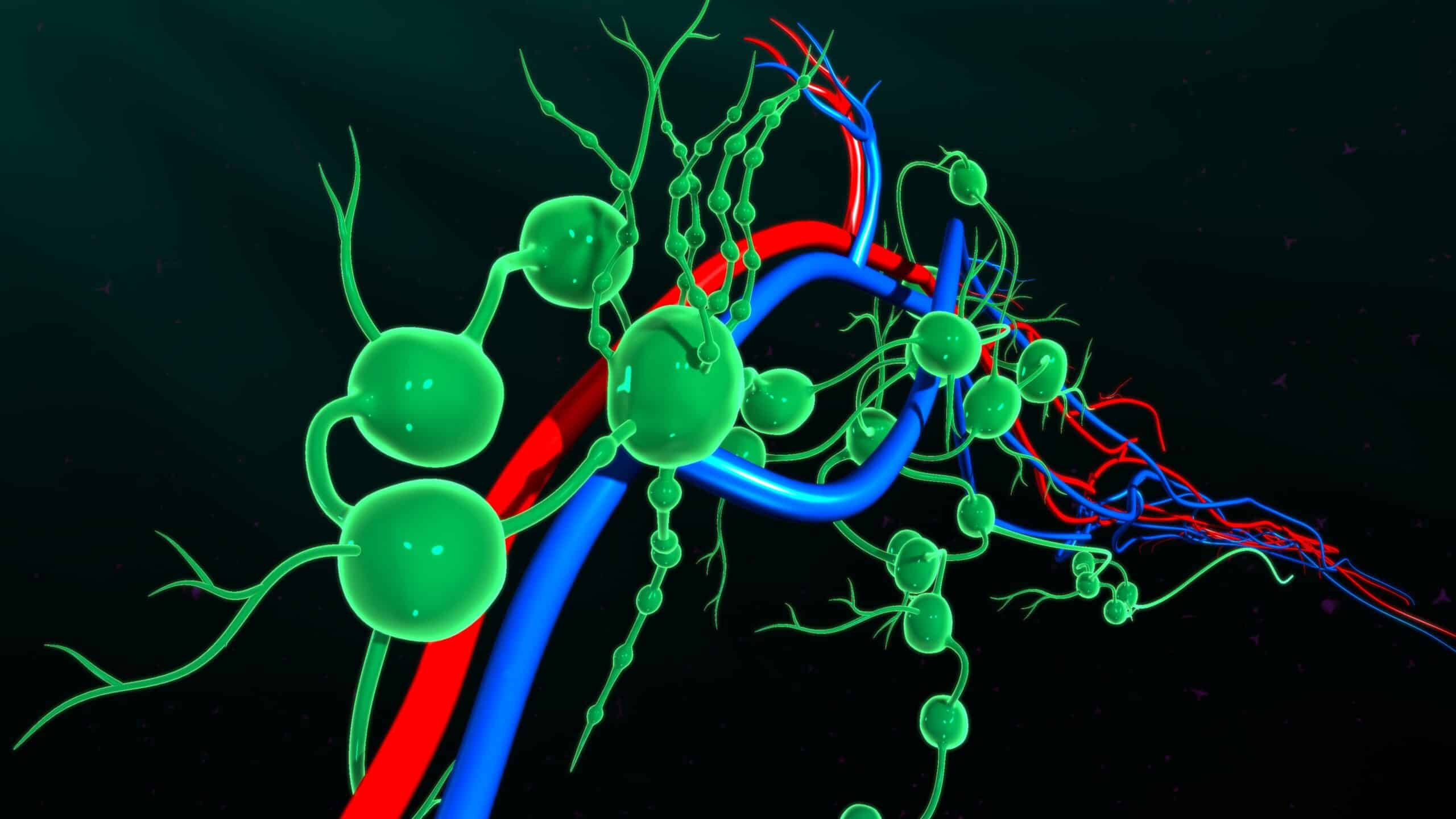
The Michigan researchers’ new drug avoided this by first being absorbed through the lymphatic system. According to lead investigator Brian Ross, a radiology professor at the University of Michigan, the lymph nodes were “sort of like a gas can that you fill up in your car. The drug is filling up this big reservoir — it’s being sequestered away from the entire body by the [lymphatic] absorption, and then slowly draining over a day into a neck vein.” This slow release helps to maintain optimal drug concentrations over time and prevents the initial blast of medicine to the system. “To my mind, it’s the world’s first kinase inhibitor that’s lymphatically absorbed,” said Ross. “It was quite astonishing, actually.”
The findings were recently published in Nature Communications. The study evaluated the effects of LP-182 on mice with myelofibrosis, a precursor to acute leukemia in which scar tissue builds up in the bone marrow. The researchers found that all mice that received the drug survived to 28 days — the planned cutoff for the study — with limited toxicity. Mice in the control group had progressive disease, “reaching humane endpoints” before 21 days. “Within the therapeutic window, we are able to maintain the on-target inhibition of two distinct pathways that are talking to one another,” said Ross in an article published on the university’s website. “This demonstrates the feasibility of delivering anti-cancer agents directly into the lymphatic system, which opens tremendous new opportunity for improving cancer therapeutic outcomes and reducing the side effects of the agents themselves,” he added.
Looking to the Future in Lymph
While Ross and his team continue to investigate how LP-182 works, they have created a new biotech firm, Lympharma, as others also work to develop cancer drugs delivered through the lymphatic system. For example, researchers from Tufts University have published a report on an mRNA cancer vaccine that is targeted to the lymph nodes and boosts T-cell response to skin cancer. Elicio Therapeutics’ Amphiphile (AMP) platform is designed to deliver peptides, proteins, and nucleic acids directly to the lymph nodes. A Phase I/II study is ongoing to evaluate Elicio’s cancer vaccine as a treatment for patients with mKRAS-driven tumors. Additionally, PureTech is developing technology to deliver drugs to the lymphatic system via an oral prodrug.
Lymphatic-delivered treatment could potentially target a broad range of cancers, including tumors, and autoimmune diseases such as lupus and multiple sclerosis. As for the drug for blood cancer Ross and his team are developing, he suggests that, optimistically, it could be in the clinic within two years.
Did you enjoy this blog post? Check out our other blog posts as well as related topics on our Webinar page.
QPS is a GLP- and GCP-compliant contract research organization (CRO) delivering the highest grade of discovery, preclinical and clinical drug research development services. Since 1995, it has grown from a tiny bioanalysis shop to a full-service CRO with 1,200+ employees in the U.S., Europe and Asia. Today, QPS offers expanded pharmaceutical contract R&D services with special expertise in neuropharmacology, DMPK, toxicology, bioanalysis, translational medicine and clinical development. An award-winning leader focused on bioanalytics and clinical trials, QPS is known for proven quality standards, technical expertise, a flexible approach to research, client satisfaction and turnkey laboratories and facilities. Through continual enhancements in capacities and resources, QPS stands tall in its commitment to delivering superior quality, skilled performance and trusted service to its valued customers. For more information, visit www.qps.com or email [email protected].