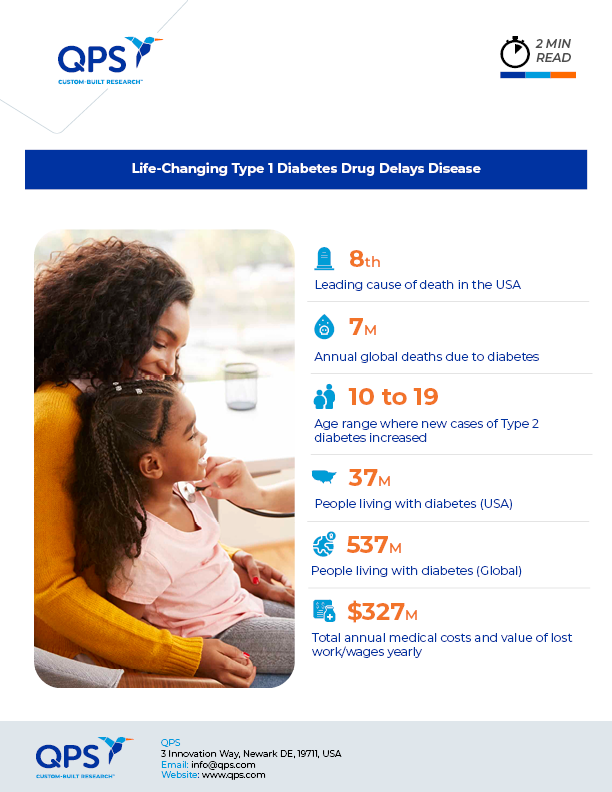
The U.S. Food and Drug Administration has approved teplizumab-mzw (TZIELD™), a drug developed by New Jersey-based Provention Bio to delay the onset of type 1 diabetes (T1D). T1D, also known as insulin-dependent, juvenile, or childhood-onset diabetes, is marked by deficient insulin production and affects an estimated 8.4 million people globally.
Teplizumab is the first and only disease-modifying treatment to delay the onset of Stage 3 T1D in adult and pediatric patients with Stage 2 T1D. The drug delayed the need for insulin shots, blood-sugar monitoring, and diet control by about two years in some patients.
T1D occurs when the immune system attacks beta cells in the pancreas, which are responsible for producing insulin. As the number of beta cells decreases, patients progress to Stage 3 T1D and become reliant on insulin injections to regulate their blood sugar levels. “This is a historic occasion for the T1D community and a paradigm shifting breakthrough for individuals aged 8 years and older with Stage 2 T1D who now have a therapy approved by the FDA to delay the onset of Stage 3 disease. It cannot be emphasized enough how precious a delay in the onset of Stage 3 T1D can be from a patient and family perspective; more time to live without and, when necessary, prepare for the burdens, complications and risks associated with Stage 3 disease” noted Ashleigh Palmer, co-founder and CEO of Provention Bio in a press release with details of the study results.
Promising Results
Teplizumab is an antibody that is administered as a daily infusion over the course of two weeks. It binds to CD3, a cell surface antigen present on T lymphocytes, and works by decreasing the activity of the immune cells that damage the beta cells.
For the clinical trial, patients with Stage 2 T1D were randomly assigned to receive teplizumab or a placebo and researchers reported the median time between randomization and diagnosis of Stage 3 T1D. This time was 50 months in the treatment group and 25 months in the placebo group, representing a statistically significant delay.
While the approval of teplizumab is an important milestone, many challenges remain before the drug can make a real difference for patients. For instance, the one-time treatment costs nearly $200,000. Getting the treatment to the right people at the right time is also a significant barrier.
To participate in the clinical trial that led to the drug’s approval, patients had to have a family member with T1D, at least two markers of the disease, and signs of blood sugar dysregulation. However, most people with T1D don’t have a family history and most children are not screened for the disease.
Finding Candidates
The origins of T1D are present in the body long before symptoms appear. Someone with two or more autoantibodies and abnormal blood sugar has a 75 percent chance of needing to rely on insulin within the next five years and a nearly 100 percent chance of it in their lifetime. A blood test can detect the warning signs during the pre-symptomatic stage. The JDRF, a T1D-focused advocacy group, is funding efforts to make these tests more accessible.
Identifying patients who could benefit from the drug could start as early as birth. First, genetic markers linked to the disease could be detected in the heel-prick test that babies receive at the hospital. Monitoring those children who carry the markers would help with early disease detection. In addition, autoantibodies can be detected with blood tests before symptoms occur. Along with blood sugar results, both types of screening could help identify at-risk patients.
Longer-Lasting Benefits?
The drug’s approval is a promising development for people with T1D, although continued effort is required to ensure that the treatment is accessible and affordable for patients. Additional research is needed to determine whether repeated treatment could extend the drug’s benefits and potentially further delay disease onset.
Did you enjoy this blog post? Check out our other blog posts as well as related topics on our Webinar page.
QPS is a GLP- and GCP-compliant contract research organization (CRO) delivering the highest grade of discovery, preclinical and clinical drug research development services. Since 1995, it has grown from a tiny bioanalysis shop to a full-service CRO with 1,100+ employees in the U.S., Europe and Asia. Today, QPS offers expanded pharmaceutical contract R&D services with special expertise in neuropharmacology, DMPK, toxicology, bioanalysis, translational medicine and clinical development. An award-winning leader focused on bioanalytics and clinical trials, QPS is known for proven quality standards, technical expertise, a flexible approach to research, client satisfaction and turnkey laboratories and facilities. Through continual enhancements in capacities and resources, QPS stands tall in its commitment to delivering superior quality, skilled performance and trusted service to its valued customers. For more information, visit www.qps.com or email info@qps.com.